Microbiome Mysteries: Solving Mental Health Puzzles
The Gut-Brain Connection: How Your Microbiome Influences Mental Health
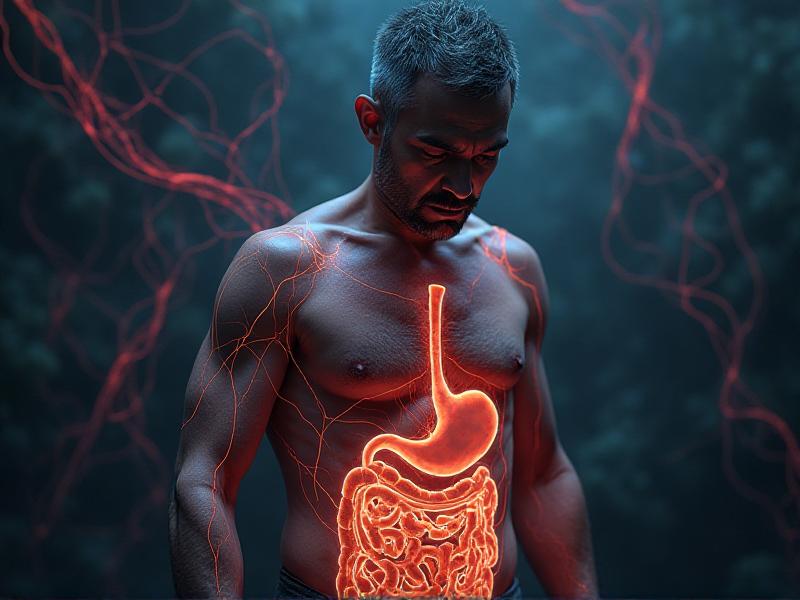
The gut has long been seen as the "second brain," and recent research is starting to find the reason. The gut microbiome, a complex ecosystem of trillions of microorganisms living in our digestive tract, plays a crucial role in regulating not just physical health but mental well-being too. Researchers have discovered that the gut and brain communicate through the gut-brain axis, a bidirectional network involving the nervous system, hormones, and immune pathways. This connection suggests that an imbalance in the gut microbiome, known as dysbiosis, could contribute to mental health disorders such as anxiety, depression, and even neurodegenerative diseases.
Studies have shown that certain gut bacteria produce neurotransmitters like serotonin and dopamine, which are essential for mood regulation. In fact, about 90% of serotonin, often called the "feel-good" hormone, is produced in the gut. When the microbiome is disrupted, it can lead to a deficiency in these critical chemicals, potentially triggering mental health issues. This revelation has opened up new avenues for treating mental health conditions by targeting the gut microbiome through diet, probiotics, and other interventions.

Understanding the gut-brain connection is just the beginning. As we delve deeper into the microbiome's mysteries, we may uncover even more ways to harness its power to improve mental health. The implications are profound, offering hope for millions of people struggling with mental health challenges.
Dysbiosis and Depression: The Microbial Link to Mood Disorders
Depression is one of the most common mental health disorders worldwide, affecting millions of people. While traditional treatments focus on addressing chemical imbalances in the brain, emerging research suggests that the gut microbiome may play a significant role in the development and progression of depression. Dysbiosis, or an imbalance in the gut microbiota, has been linked to increased inflammation, which is a known contributor to depressive symptoms.
Studies have found that individuals with depression often have a less diverse gut microbiome compared to healthy individuals. Specific bacterial strains, such as Lactobacillus and Bifidobacterium , are often reduced in people with depression. These bacteria are known to produce short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and support brain health. When these beneficial bacteria are diminished, it can lead to a cascade of negative effects, including increased gut permeability (leaky gut) and systemic inflammation, both of which are associated with depression.

This microbial link to depression opens up exciting possibilities for treatment. Probiotics, prebiotics, and dietary changes aimed at restoring gut balance are being explored as complementary therapies for depression. While more research is needed, the potential to address mental health through the gut is a promising frontier.
Anxiety and the Microbiome: Can Gut Bacteria Calm the Mind?
Anxiety disorders are among the most prevalent mental health conditions, affecting nearly one in five adults. While the exact causes of anxiety are complex and multifaceted, the gut microbiome is emerging as a key player in regulating stress and anxiety levels. The gut-brain axis, which facilitates communication between the gut and the brain, is heavily influenced by the microbiome. When this axis is disrupted, it can lead to heightened stress responses and anxiety.
Research has shown that certain gut bacteria can produce gamma-aminobutyric acid (GABA), a neurotransmitter that helps calm the nervous system. Low levels of GABA are associated with anxiety, and boosting its production through gut bacteria could offer a natural way to alleviate symptoms. Additionally, studies on animals have demonstrated that transplanting gut bacteria from anxious individuals into germ-free mice can induce anxiety-like behaviors, further highlighting the microbiome's role in mental health.

These findings suggest that targeting the gut microbiome could be an effective strategy for managing anxiety. Probiotics, fermented foods, and stress-reducing practices like mindfulness and yoga may help restore balance to the gut and, in turn, calm the mind. As we continue to explore this connection, the potential for microbiome-based therapies to transform mental health care grows.
The Role of Diet in Shaping a Healthy Microbiome
What we eat has a profound impact on the composition and function of our gut microbiome. A diet rich in fiber, fruits, vegetables, and fermented foods promotes the growth of beneficial bacteria, while a diet high in processed foods, sugar, and unhealthy fats can lead to dysbiosis. The Western diet, in particular, has been linked to a less diverse microbiome and an increased risk of mental health disorders.
Fiber, found in plant-based foods, is especially important for gut health. It serves as a prebiotic, feeding the beneficial bacteria in the gut and helping them produce SCFAs, which have anti-inflammatory and neuroprotective effects. On the other hand, diets high in sugar and saturated fats can promote the growth of harmful bacteria, leading to inflammation and a weakened gut barrier. This, in turn, can negatively affect the gut-brain axis and contribute to mental health issues.

Adopting a microbiome-friendly diet is one of the most effective ways to support mental health. Incorporating more whole, unprocessed foods and reducing the intake of sugar and unhealthy fats can help create a balanced and diverse microbiome. As research continues to uncover the intricate relationship between diet, the microbiome, and mental health, the old adage "you are what you eat" takes on new meaning.
Probiotics and Psychobiotics: The Future of Mental Health Treatment?
Probiotics, live bacteria that confer health benefits when consumed, have long been associated with gut health. However, recent research suggests that certain strains of probiotics, known as psychobiotics, may also have a positive impact on mental health. These psychobiotics can influence the gut-brain axis by producing neurotransmitters, reducing inflammation, and strengthening the gut barrier.
Clinical trials have shown promising results for psychobiotics in alleviating symptoms of anxiety and depression. For example, a study published in the journal Gastroenterology found that participants who took a specific probiotic strain experienced reduced anxiety and improved mood compared to those who took a placebo. While the field is still in its early stages, the potential for psychobiotics to complement traditional mental health treatments is immense.
As we continue to explore the microbiome's role in mental health, psychobiotics could become a cornerstone of treatment. However, it's important to note that not all probiotics are created equal, and more research is needed to identify the most effective strains and dosages. For now, incorporating probiotic-rich foods like yogurt, kefir, and sauerkraut into your diet is a simple way to support both gut and mental health.
The Microbiome and Neurodegenerative Diseases: A New Frontier
While much of the research on the microbiome and mental health has focused on mood disorders, scientists are also investigating its role in neurodegenerative diseases like Alzheimer's and Parkinson's. These conditions are characterized by the progressive loss of neurons and cognitive function, and emerging evidence suggests that the gut microbiome may play a role in their development and progression.
Studies have found that individuals with Alzheimer's disease often have a less diverse gut microbiome and higher levels of harmful bacteria. These bacteria can produce toxins that contribute to inflammation and the formation of amyloid plaques, a hallmark of Alzheimer's. Similarly, in Parkinson's disease, researchers have observed changes in the gut microbiome that may influence the progression of motor symptoms.

This research opens up new possibilities for preventing and treating neurodegenerative diseases by targeting the gut microbiome. Interventions like probiotics, dietary changes, and fecal microbiota transplantation (FMT) are being explored as potential therapies. While the field is still in its infancy, the microbiome's role in brain health is an exciting area of study that could revolutionize how we approach these devastating conditions.
Stress and the Microbiome: A Vicious Cycle
Stress is an inevitable part of life, but chronic stress can take a toll on both the mind and the body. One of the ways stress affects us is by disrupting the gut microbiome. When we're stressed, our bodies release cortisol, a hormone that can alter the composition of the gut microbiota. This, in turn, can lead to increased gut permeability, inflammation, and a weakened immune system.
Interestingly, the relationship between stress and the microbiome is bidirectional. Just as stress can disrupt the microbiome, an imbalanced microbiome can also exacerbate stress. This creates a vicious cycle where stress and dysbiosis feed off each other, leading to a decline in both physical and mental health. Breaking this cycle is essential for maintaining overall well-being.
Managing stress through mindfulness, exercise, and a healthy diet can help restore balance to the gut microbiome. Additionally, probiotics and prebiotics may offer support by promoting the growth of beneficial bacteria. By addressing both stress and the microbiome, we can take a holistic approach to improving mental and physical health.
The Future of Microbiome Research: What Lies Ahead?
The field of microbiome research is still in its early stages, but the discoveries made so far have already transformed our understanding of mental health. As technology advances, scientists are able to study the microbiome in greater detail, uncovering new connections and potential therapies. From personalized probiotics to microbiome-based diagnostics, the possibilities are endless.
One of the most exciting areas of research is the development of microbiome-based treatments for mental health disorders. These treatments could include targeted probiotics, dietary interventions, and even fecal microbiota transplantation (FMT). As we continue to unravel the mysteries of the microbiome, we may find that the key to solving some of the most complex mental health puzzles lies within our own bodies.

The future of microbiome research holds immense promise for improving mental health and overall well-being. By continuing to explore this fascinating field, we can unlock new ways to heal the mind and body, offering hope to millions of people around the world.