Microbial Messengers: Decoding the Anxiety-Gut Connection
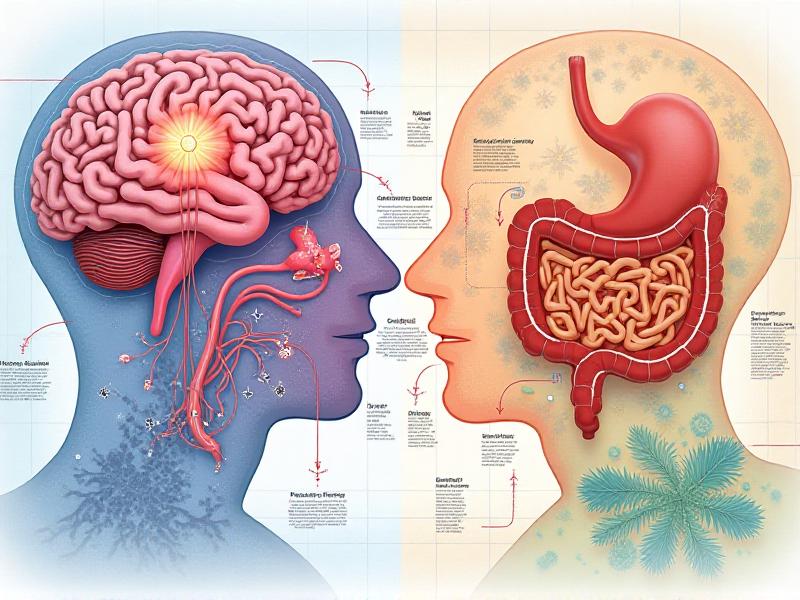
The Gut-Brain Axis: A Two-Way Communication Highway
The gut-brain axis is a complex, bidirectional communication network that links the emotional and cognitive centers of the brain with peripheral intestinal functions. This intricate system involves neural, hormonal, and immunological signaling pathways. The gut, often referred to as the "second brain," houses millions of neurons and produces a significant amount of neurotransmitters, such as serotonin, which play a crucial role in mood regulation. Emerging research suggests that the gut microbiota—the trillions of microorganisms residing in our digestive tract—acts as a key mediator in this communication. These microbial messengers influence brain function and behavior, including anxiety and stress responses.
The vagus nerve, a major component of the parasympathetic nervous system, serves as a direct line of communication between the gut and the brain. Studies have shown that gut microbes can stimulate the vagus nerve, sending signals to the brain that affect mood and emotional states. For instance, certain strains of bacteria, such as Lactobacillus and Bifidobacterium , have been found to reduce anxiety-like behaviors in animal models. This highlights the potential of microbial interventions in managing anxiety disorders.

Microbial Metabolites: The Chemical Language of the Gut
The gut microbiota produces a wide array of metabolites that serve as chemical messengers, influencing both local and systemic processes. Short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate, are among the most well-studied microbial metabolites. These compounds are produced through the fermentation of dietary fibers and have been shown to exert anti-inflammatory and neuroprotective effects. Butyrate, in particular, has been linked to improved brain function and reduced anxiety by enhancing the integrity of the blood-brain barrier and promoting the production of brain-derived neurotrophic factor (BDNF).
In addition to SCFAs, gut microbes also produce neurotransmitters and neuromodulators, such as gamma-aminobutyric acid (GABA) and serotonin. GABA, the primary inhibitory neurotransmitter in the brain, plays a key role in reducing neuronal excitability and promoting relaxation. Interestingly, certain gut bacteria can synthesize GABA, potentially influencing anxiety levels. Similarly, about 90% of the body's serotonin is produced in the gut, underscoring the importance of microbial activity in mood regulation.

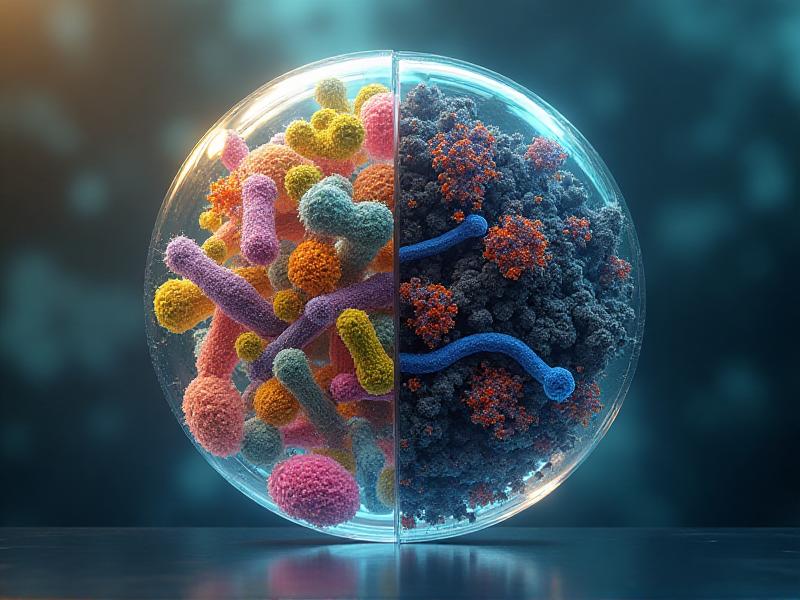
Dysbiosis and Anxiety: When the Microbial Balance is Disrupted
Dysbiosis, an imbalance in the gut microbiota, has been increasingly linked to mental health disorders, including anxiety. Factors such as poor diet, stress, antibiotics, and infections can disrupt the delicate equilibrium of the gut microbiome, leading to an overgrowth of harmful bacteria and a reduction in beneficial species. This imbalance can trigger inflammation, alter neurotransmitter production, and impair the gut-brain axis, contributing to anxiety symptoms.
Research has shown that individuals with anxiety disorders often exhibit distinct microbial profiles compared to healthy controls. For example, reduced levels of Lactobacillus and Bifidobacterium have been observed in people with anxiety, while increased levels of pro-inflammatory bacteria, such as Enterobacteriaceae , are associated with heightened anxiety and stress. These findings suggest that restoring microbial balance through dietary interventions, probiotics, or fecal microbiota transplantation could be a promising approach to managing anxiety.
Probiotics and Psychobiotics: Harnessing Microbes for Mental Health
Probiotics, live microorganisms that confer health benefits when consumed in adequate amounts, have gained attention for their potential to improve mental health. Specific strains of probiotics, known as psychobiotics, have been shown to reduce anxiety and depression by modulating the gut-brain axis. For instance, Lactobacillus rhamnosus and Bifidobacterium longum have demonstrated anxiolytic effects in both animal and human studies.
The mechanisms underlying the benefits of psychobiotics are multifaceted. They include the production of neurotransmitters, reduction of inflammation, and enhancement of the gut barrier function. Additionally, psychobiotics can influence the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body's stress response. By modulating the HPA axis, these beneficial microbes can help mitigate the physiological and psychological effects of stress, offering a natural and holistic approach to anxiety management.

Diet and the Microbiome: Feeding Your Gut, Calming Your Mind
Diet plays a pivotal role in shaping the gut microbiome and, by extension, mental health. A diet rich in fiber, fermented foods, and polyphenols promotes the growth of beneficial bacteria, while a diet high in processed foods, sugar, and saturated fats can lead to dysbiosis. The Mediterranean diet, for example, has been associated with a diverse and balanced microbiome, as well as reduced anxiety and depression rates.
Prebiotics, non-digestible fibers that serve as food for beneficial gut bacteria, are particularly important for maintaining microbial health. Foods such as garlic, onions, bananas, and asparagus are rich in prebiotics and can help support a healthy gut-brain axis. Additionally, fermented foods like yogurt, kefir, sauerkraut, and kimchi introduce live probiotics into the gut, further enhancing microbial diversity and resilience. By making mindful dietary choices, individuals can nurture their gut microbiome and, in turn, support their mental well-being.

The Future of Microbial Medicine: Personalized Approaches to Anxiety
As our understanding of the gut-brain axis deepens, the potential for personalized microbial medicine becomes increasingly apparent. Advances in microbiome sequencing and artificial intelligence are paving the way for tailored interventions that target an individual's unique microbial profile. For example, microbiome-based diagnostics could identify specific imbalances associated with anxiety, enabling the development of customized probiotic formulations or dietary recommendations.
Moreover, the integration of microbial therapies with other treatment modalities, such as cognitive-behavioral therapy (CBT) and pharmacotherapy, holds promise for more comprehensive and effective anxiety management. By addressing both the microbial and psychological aspects of anxiety, these integrative approaches could revolutionize mental health care. As research continues to unravel the complexities of the gut-brain connection, the future of microbial medicine offers hope for those struggling with anxiety and other mental health challenges.