Bacteria, Brains, and Breakthroughs: A New Mental Health Paradigm
The Gut-Brain Axis: How Bacteria Influence Mental Health
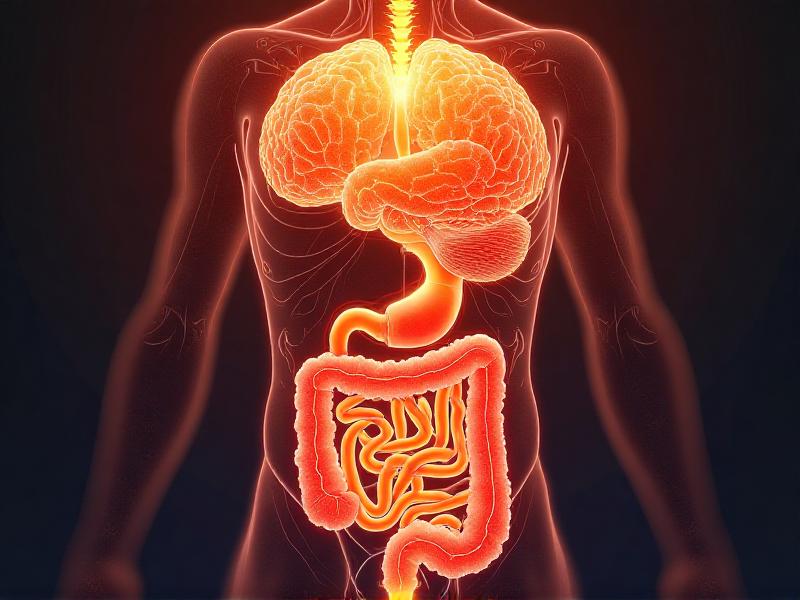
For decades, the brain was considered the sole commander of our mental health. However, recent research has uncovered a fascinating connection between the gut and the brain, often referred to as the gut-brain axis. This bidirectional communication system involves the central nervous system, the enteric nervous system, and the trillions of microorganisms residing in our gut, collectively known as the gut microbiota.
Studies have shown that the gut microbiota can produce neurotransmitters like serotonin and dopamine, which are crucial for regulating mood and behavior. In fact, approximately 90% of serotonin, often dubbed the "happiness hormone," is produced in the gut. This discovery has led scientists to explore how imbalances in gut bacteria, known as dysbiosis, may contribute to mental health disorders such as anxiety, depression, and even autism spectrum disorders.
Emerging evidence suggests that probiotics, prebiotics, and dietary changes can positively influence the gut-brain axis, offering new avenues for mental health treatment. For instance, a diet rich in fiber, fermented foods, and omega-3 fatty acids has been linked to improved gut health and reduced symptoms of depression. These findings are reshaping our understanding of mental health, emphasizing the importance of a holistic approach that considers the gut as a key player in emotional well-being.
The Microbiome and Neuroplasticity: Rewiring the Brain
Neuroplasticity, the brain's ability to reorganize itself by forming new neural connections, is a cornerstone of mental health. It allows us to adapt to new experiences, recover from injuries, and learn new skills. Recent research has revealed that the gut microbiome plays a significant role in this process, influencing brain structure and function.
Certain gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, which have been shown to promote neurogenesis—the growth of new neurons—and enhance synaptic plasticity. These effects are particularly important in conditions like depression and PTSD, where neuroplasticity is often impaired. By modulating the gut microbiome, scientists believe it may be possible to enhance the brain's ability to heal and adapt.
Animal studies have provided compelling evidence for this connection. For example, mice raised in sterile environments, devoid of gut bacteria, exhibit reduced neuroplasticity and increased anxiety-like behaviors. When these mice are colonized with healthy gut bacteria, their brain function and behavior improve significantly. These findings suggest that maintaining a healthy microbiome could be a powerful strategy for supporting mental health and cognitive function.

Inflammation and Mental Health: The Hidden Link
Chronic inflammation has long been associated with physical health conditions like heart disease and diabetes. However, recent studies have uncovered a surprising link between inflammation and mental health disorders. The gut microbiome plays a central role in regulating the body's inflammatory response, and imbalances in gut bacteria can lead to systemic inflammation that affects the brain.
Inflammatory molecules like cytokines can cross the blood-brain barrier, disrupting neurotransmitter function and contributing to symptoms of depression and anxiety. This has led researchers to explore anti-inflammatory treatments, such as omega-3 supplements and anti-inflammatory diets, as potential interventions for mental health disorders.
One groundbreaking study found that individuals with depression who also had high levels of inflammation were less responsive to traditional antidepressants. However, when these patients were treated with anti-inflammatory drugs, their symptoms improved significantly. This suggests that addressing inflammation could be a key component of personalized mental health care, offering hope for those who have not benefited from conventional treatments.
Probiotics and Psychobiotics: The Future of Mental Health Treatment
As the connection between the gut and the brain becomes clearer, researchers are exploring the potential of probiotics and psychobiotics—live bacteria that confer mental health benefits—as novel treatments for psychiatric disorders. These microorganisms can influence brain function by producing neurotransmitters, reducing inflammation, and enhancing the gut barrier.
Several clinical trials have shown promising results. For example, a study involving patients with major depressive disorder found that those who took a specific strain of probiotic experienced significant improvements in mood compared to the placebo group. Similarly, probiotics have been shown to reduce symptoms of anxiety and improve cognitive function in healthy individuals.
While the field is still in its infancy, the potential of psychobiotics is immense. Researchers are working to identify the most effective strains and develop targeted formulations for specific mental health conditions. In the future, psychobiotics could become a standard part of mental health treatment, offering a natural and non-invasive alternative to traditional therapies.

The Role of Diet in Shaping the Gut-Brain Connection
Diet is one of the most powerful tools we have for influencing the gut microbiome and, by extension, mental health. The foods we eat can either promote the growth of beneficial bacteria or contribute to dysbiosis, leading to a cascade of negative effects on the brain.
A diet high in processed foods, sugar, and unhealthy fats has been linked to an increased risk of depression and anxiety. In contrast, a diet rich in whole foods, fiber, and fermented products supports a diverse and balanced microbiome, which is associated with better mental health outcomes. The Mediterranean diet, for example, has been shown to reduce symptoms of depression and improve cognitive function.
Emerging research also highlights the importance of personalized nutrition. Genetic factors, lifestyle, and even geographic location can influence how individuals respond to different diets. By tailoring dietary recommendations to an individual's unique microbiome, it may be possible to optimize mental health and prevent psychiatric disorders.

Stress, the Microbiome, and Mental Resilience
Stress is an inevitable part of life, but chronic stress can take a toll on both the gut and the brain. When we experience stress, the body releases cortisol, a hormone that can disrupt the balance of gut bacteria and weaken the gut barrier. This, in turn, can lead to inflammation and negatively impact mental health.
However, the relationship between stress and the microbiome is bidirectional. A healthy gut microbiome can enhance resilience to stress by regulating the hypothalamic-pituitary-adrenal (HPA) axis, which controls the body's stress response. Certain strains of gut bacteria have been shown to reduce cortisol levels and promote a sense of calm.
Mind-body practices like meditation, yoga, and deep breathing have been found to support a healthy microbiome and improve mental resilience. These practices not only reduce stress but also promote the growth of beneficial bacteria, creating a positive feedback loop that enhances overall well-being.

Breaking the Stigma: A New Approach to Mental Health
The traditional approach to mental health has often focused on treating symptoms with medication and therapy. While these methods are valuable, they do not address the underlying biological factors that contribute to mental health disorders. The emerging paradigm of gut-brain health offers a more comprehensive and holistic approach, emphasizing the importance of diet, lifestyle, and the microbiome.
By shifting the focus from the brain to the gut, we can break the stigma surrounding mental health and encourage a more proactive approach to well-being. This new perspective empowers individuals to take control of their mental health through simple, everyday choices like eating a balanced diet, managing stress, and incorporating probiotics into their routine.
As research continues to uncover the intricate connections between bacteria, brains, and breakthroughs, we are on the brink of a mental health revolution. This paradigm shift has the potential to transform how we understand, treat, and prevent mental health disorders, offering hope for a healthier and happier future.










